Point-of-care testing: A winning strategy in the battle against diabetes
Wednesday, September 07, 2022
by Susan Garramone, Senior Clinical Marketing Manager - Siemens Healthineers
Diabetes: The medical condition
Diabetes is a chronic, metabolic disease characterized by elevated levels of blood glucose. The hormone insulin is required for glucose to enter the body’s cells, where it is used for energy. If the body does not make enough insulin (type 1 diabetes) or does not respond to insulin as it should (type 2 diabetes), the level of glucose in the blood becomes elevated.1 This high blood sugar, or hyperglycemia, is dangerous and can lead to long-term complications.1,2
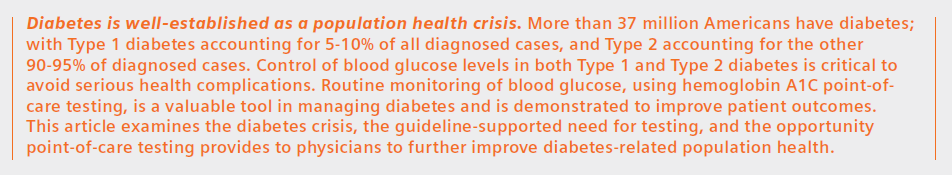
Type 1 diabetes is an autoimmune condition typically diagnosed in children, teens, and young adults.1 There is no cure for type 1 diabetes, and in addition to following a healthy eating and exercise plan, people with type 1 diabetes need to take insulin every day to control blood glucose levels.3
Type 2 diabetes, representing the majority of diabetes diagnoses, is a condition that develops over time.1,3 Once more commonly diagnosed in adults, the prevalence of diabetes in children, teens, and young adults is increasing.1 Lifestyle management, with healthy eating and exercise, is a cornerstone of type 2 diabetes treatment plans. Additionally, patients may be prescribed insulin or other injectable or oral diabetes medications to help manage blood sugar.1
Diabetes: The comorbidity concern
Not only is diabetes the seventh-leading cause of death in the United States, affecting 11.3% of the U.S. population, it also is attributed to an estimated $327 billion in annual medical and lost productivity costs.3-6 Generally, care for patients with diabetes accounts for 1 in 4 healthcare dollars spent in the U.S., and a large portion of these costs results from diabetes-associated comorbidities that include potential neurological, cardiovascular, renal, and other chronic complications.2 A search of the PubMed National Library of Medicine yields thousands of new publications on diabetes and diabetes-related issues thus far in 2022, underscoring the importance of this chronic disease and the efforts to help those affected.7
Similarly, the body of evidence regarding the profound consequences of diabetes continues to grow.
The results also showed that for all chronic conditions, the average age of onset among people with type 2 diabetes was 5 years earlier than in people without the disease.8
Another recent study by Antal et al. reports type 2 diabetes mellitus (T2DM) is associated with neurocognitive changes suggestive of accelerated brain aging and cognitive decline.9
The wide-reaching consequences of diabetes and importance of diabetes management were devastatingly evident during the COVID-19 pandemic, when reports emerged demonstrating that COVID-19 was the leading cause of death in people with diabetes in the fourth quarter of 2020.10
In fact, a large systematic review and meta-analysis conducted by researchers from the University of Aberdeen has found that people with diabetes are almost twice as likely to die with COVID-19, and almost three times as likely to be critically or severely ill, compared to those without the condition.11 They reported that HbA1c over 70 mmol (equivalent to 8.6% HbA1c) increased the risk of mortality among patients with diabetes.
Additionally, at the 2022 American Diabetes Association meeting, a presentation by Harding et al. identified that diabetes may increase the risk for long COVID symptoms four-fold. In fact, the author was quoted as stating, “Careful monitoring of glucose levels in at-risk individuals may help to mitigate excess risk and reduce the burden of lingering symptoms that inhibit their overall well-being.”12

- https://www.practiceupdate.com/content/ada-diabetes-may-quadruple-risk-for-long-covid/137205/23/8/2. Accessed 6-21-22.
- https://www.healthcatalyst.com/insights/managing-diabetes-population-health-management. Accessed 6-21-22.
Diabetes: Monitoring leads to management
It is quite clear that people with diabetes are at risk for poor health outcomes, and diabetes management is critical. The higher a patient’s hemoglobin A1c level, the poorer their blood sugar control and the higher their risk of complications.15 For example, 1 out of 3 adults with diabetes develop diabetic kidney disease, which can then lead to high blood pressure, heart disease, stroke, and early death.16
However, it is also quite clear that facilitating changes in patient behavior, with diabetes self-management education and patient-provider collaboration as outlined by the ADA, can improve health outcomes.17 In fact, studies have shown that every percentage-point drop in A1c blood test results can reduce the risk of eye, nerve, and kidney disease complications by as much as 40%.18,19 Even with this knowledge, high HbA1c levels are seen in 50–60% of diabetic patients, indicating that they either are not receiving proper care or are not adhering to their treatment regimen!20

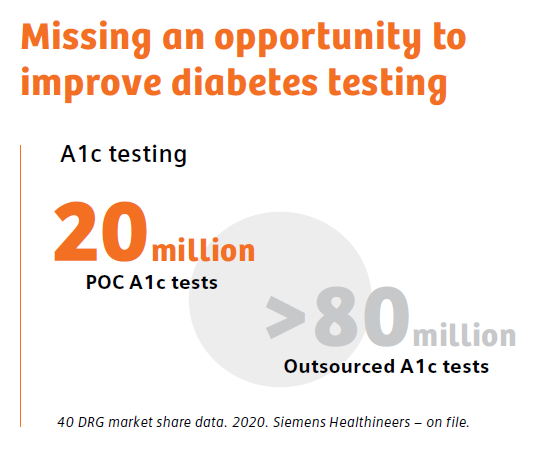
Guidelines call for routine testing of hemoglobin A1c (HbA1c) and urine albumin-creatinine ratio (uACR) for diabetes and chronic kidney disease monitoring and management, respectively.21,22 These tests are part of national quality measures, which underscores their importance in early diagnosis, monitoring, and treatment leading to improved outcomes. However, there is a major disconnect: Adherence to recommended testing is astonishingly low—only approximately 70% and 32% of patients with diabetes follow the testing guidelines for HbA1c and uACR, respectively.23,24
Reasons for low test adherence were addressed in a 2021 study by Al Hayek et al. in which patients identified having to make a trip to a laboratory as a main barrier to testing.25 Patient-reported pain points included “difficulties in handling absence from school/work (56%), inconvenience associated with revisits (45.3%), and the additional costs of travel (44%)”.25 Additionally, a review by Schnell et al. documented the potential for time delays in pre-visit laboratory HbA1c testing.26 These delays may lead to nonadherence, downstream delays in communicating results and intensifying or modifying treatment, and reduced patient adherence to the treatment plan.
Diabetes: Primary care holds the key to control
Did you know that having a primary-care doctor, as well as getting routine care and health-screening services, are linked to improved overall health and longevity?27
Primary-care physicians treat at least 90% of patients with diabetes in the United States. Therefore, the biggest opportunity for positive change lies within the primary-care office.28
According to the ADA, “The goals of diabetes treatment are to prevent or delay complications, optimize quality of life, and establish a care plan with patients based on their individual preferences, principles, and goals.”29 Implementation of point-of-care testing in the primary-care office provides an opportunity to meet these goals, whereby patient education and monitoring of progress with real-time clinical data, such as guideline-driven HbA1c and uACR results, can increase patient motivation to make lifestyle modifications and adhere to medication-management plans. In fact, in 2021 the ADA stated that POC testing for A1c provides opportunity for more timely treatment changes.21
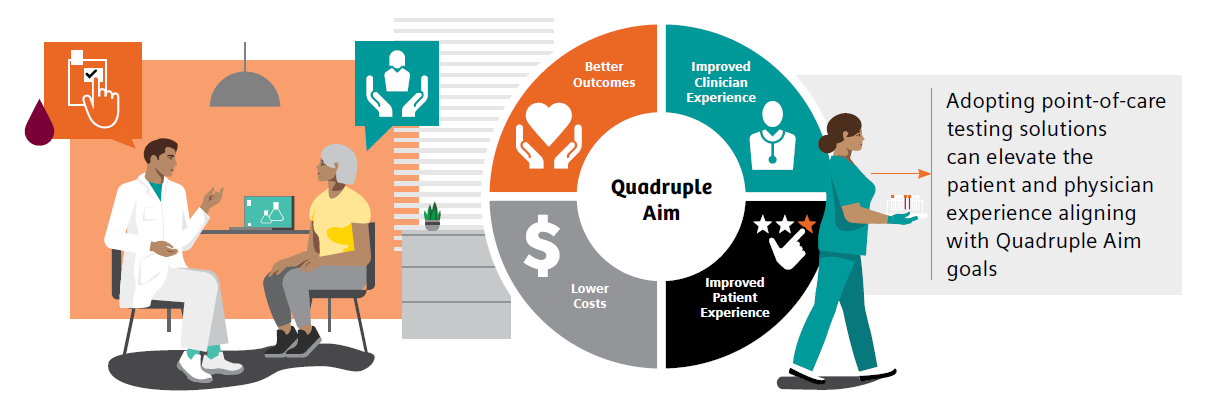
There is a large body of evidence further supporting the clinical value of point-of-care testing (POCT) as a quick, easy, reliable method for monitoring diabetes in the primary-care office setting. Such testing can improve test adherence and patient outcomes while also increasing practice efficiency, decreasing costs, and driving achievement of quality measures.25,30-36 In addition, studies have demonstrated that POCT is associated with a high level of patient and staff satisfaction, which further aligns with the Quadruple-Aim goals of better outcomes, lower costs, improved patient experience, and improved clinician experience.25,30,31,36
Diabetes: The clinical conundrum
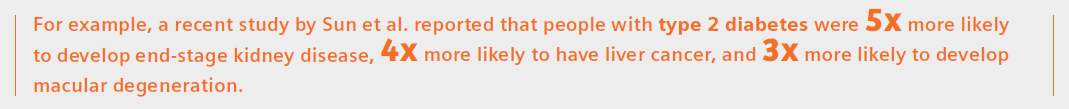
There are a lot of knowns when discussing diabetes.
The review by Schnell et al. neatly summarizes the benefits of diabetes testing at the point of care:26
- Increases compliance with recommendations for HbA1c testing frequency and treatment adoption
- Improves clinical outcomes
- Facilitates patient education and motivation
- Improves patient’s quality of life
- Appears to contribute to cost/time savings both for healthcare professionals and patients
That describes a winning strategy for facilitating positive change in the battle against diabetes—a win for patients, and a win for the physicians who care for them. If point-of-care, in-office diabetes testing is not a tool currently in your diabetes-management tool kit, perhaps it is time for its adoption.
References
- https://www.cdc.gov/diabetes/basics/diabetes.html. Accessed 6-21-22.
- https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html. Accessed 6-21-22.
- https://www.cdc.gov/diabetes/library/socialmedia/infographics/diabetes.html. Accessed 6-21-22.
- https://www.cdc.gov/diabetes/basics/quick-facts.html. Accessed 6-21-22.
- https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed 6-21-22.
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-28. doi: 10.2337/dci18-0007. Accessed 6-21-22.
- gov. (diabetes) and (2022) Search. Accessed 6/15/22.
- https://www.medscape.co.uk/viewarticle/burden-chronic-conditions-heavier-type-2-diabetes-2022a1000tht. Diabetes UK Professional Conference 2022: Abstract A19 (P139). Presented March 29. Accessed 6/15/22.
- Antal B, McMahon LP, Sultan SF, Lithen A, Wexler DJ, Dickerson B, Ratai E-M, Mujica-Parodi LR. Type 2 diabetes mellitus accelerates brain aging and cognitive decline: complementary findings from UK Biobank and meta-analyses. eLife. 2022;11:e73138. https://doi.org/10.7554/eLife.73138
- https://www.healio.com/news/endocrinology/20220517/covid19-leading-cause-of-death-in-people-with-diabetes-in-fourth-quarter-of-2020. Accessed 6-21-22.
- Kastora S, Patel M, Carter B, Delibegovic M, Myint PK. Impact of diabetes on COVID-19 mortality and hospital outcomes from a global perspective: an umbrella systematic review and meta-analysis. Endocrinol Diabetes Metab. 2022 May;5(3):e00338. doi: 10.1002/edm2.338. Epub 2022 Apr 20. PMID: 35441801; PMCID: PMC9094465.
- https://www.practiceupdate.com/content/ada-diabetes-may-quadruple-risk-for-long-covid/137205/23/8/2. Accessed 6-21-22.
- https://www.ajmc.com/view/multiple-chronic-conditions-in-type-2-diabetes-mellitus-prevalence-and-consequences. Accessed 6-27-22.
- https://www.verywellhealth.com/side-effects-of-diabetes-5181506. Accessed 6-27-22.
- https://www.healthcatalyst.com/insights/managing-diabetes-population-health-management. 6-27-22.
- https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html. Accessed 6-27-22.
- https://diabetesjournals.org/care/article/43/Supplement_1/S48/30785/5-Facilitating-Behavior-Change-and-Well-being-to. Accessed 6-27-22.
- Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C: Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993 Sep 30;329(14):977-86.
- https://www.cdc.gov/chronicdisease/programs-impact/pop/diabetes.htm. Accessed 6-22-22.
- LeBlanc ES, Rosales AG, Kachroo S, et al. Provider beliefs about diabetes treatment have little impact on glycemic control of their patients with diabetes. BMJ Open Diabetes Res Care. 2015;3:e000062. https://doi.org/10.1136/bmjdrc-2014-000062.
- American Diabetes Association. Glycemic targets: standards of medical care in diabetes—2021. Diabetes Care. 2021 Jan;44(Suppl 1):S73-S84. Available from: https://doi.org/10.2337/dc21-S006.
- American Diabetes Association Professional Practice Committee, et al. Chronic kidney disease and risk management: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl_1):S175-S184. doi:10.2337/dc22-S011.
- https://www.cdc.gov/diabetes/pdfs/library/Diabetes-Report-Card-2019-508.pdf. Accessed 12-17-21. Accessed 6-22-22.
- Alfego D, et al. Chronic kidney disease testing among at-risk adults in the U.S. remains low: real-world evidence from a national laboratory database. Diabetes Care. 2021;44(9):2025-32. doi:10.2337/dc21-0723.
- Al Hayek AA, et al. Assessment of patient satisfaction with on-site point-of-care hemoglobin A1c testing: an observational study. Diabetes Ther. 2021;12(9):2531-44. doi: 10.1007/s13300-021-01126-7
- Schnell O, et al. Impact of HbA1c testing at point of care on diabetes management. J Diabetes Sci Technol. 2017;11(3):611-17. doi: 10.1177/1932296816678263
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179(4):506-14. doi: 10.1001/jamainternmed.2018.7624
- Davidson JA. The increasing role of primary care physicians in caring for patients with type 2 diabetes mellitus. Mayo Clinic proceedings. 2010;85(12 Suppl):S3-4. doi: 10.4065/mcp.2010.0466
- American Diabetes Association. Standards of Medical Care in Diabetes—2022 Abridged for Primary Care Providers. Clin Diabetes. 2022 Jan 1;40(1):10-38. https://doi.org/10.2337/cd22-as01
- Crocker JB, et al. The impact of point-of-care hemoglobin A1c testing on population health-based onsite testing adherence: a primary-care quality improvement study. J Diabetes Sc Technol. 2021;15(3):561-7. doi: 10.1177/1932296820972751.
- Crocker JB, Lee-Lewandrowsky E, Lewandrowsky N, et al. Implementation of point-of-care testing in an ambulatory practice of an academic medical center. Am J Clin Pathol. 2014;142(5):640-6.
- Christofides EA, Desai N. Optimal early diagnosis and monitoring of diabetic kidney disease in type 2 diabetes mellitus: addressing the barriers to albuminuria testing. J Prim Care Community Health. 2021;12:21501327211003683. doi: 10.1177/21501327211003683.
- Schultes B, Emmerich S, Kistler AD, Mecheri B, Schnell O, Rudofsky G. Impact of albumin-to-creatinine ratio point-of-care testing on the diagnosis and management of diabetic kidney disease. J Diabetes Sci Technol. 2021 Oct 28;19322968211054520. doi: 10.1177/19322968211054520.
- Rhyu J, Lambrechts S, Han MA, Freeby MJ. Utilizing point-of-care A1c to impact outcomes – can we make it happen in primary care? Curr Opin Endocrinol Diabetes Obes. 2022 Feb 1;29(1):29-33. doi: 10.1097/MED.0000000000000700.
- Nichols JH. Utilizing point-of-care testing to optimize patient care. EJIFCC. 2021 Jun;32(2):140-4.
- Crocker B, Lewandrowski EL, Lewandrowski N, Gregory K, Lewandrowski K. Patient satisfaction with point-of-care laboratory testing: report of a quality improvement program in an ambulatory practice of an academic medical center. Clin Chim Acta. 2013 Sep 23;424:8-11. doi: 10.1016/j.cca.2013.04.025. Epub 2013 May 10. PMID: 23669184.
- https://www.cdc.gov/nchs/fastats/kidney-disease.htm. Accessed 6-22-22.
- https://www.kidney.org/atoz/content/does-type-2-diabetes-increase-your-risk-kidney-disease-yes. Accessed 6-27-22.
- https://www.medicaid.gov/state-overviews/scorecard/comprehensive-diabetes-care/index.html. Accessed 6-27-22.
- https://www.kff.org/other/state-indicator/total-active-physicians/. Accessed 6-22-22.
- DRG market share data. Siemens Healthcare Diagnostics Inc. (on file). 2020.

